Welcome to this Quarter’s Product Pulse
Q3 2025 Product Newsletter
This quarter, we’re delivering a powerful lineup of product enhancements that make member experiences more seamless, personalized, and high impact. From smarter navigation tools and AI-powered support to real-time configuration and deep linking capabilities, these updates are designed to reduce friction, boost engagement, and give clients greater control – all while driving measurable outcomes across the platform.
Powering Your Competitive Edge in the ASO Market
Available NowAs employer demands grow, health plans are expected to deliver more than just benefits. Today’s market requires a seamless, unified experience that brings together care navigation, benefits guidance, and wellness, all in one place. At the same time, plans must demonstrate ROI, reduce costs, and keep employees engaged and satisfied.
Pager Health’s ASO solution helps plans deliver the solution your employers want.
- Fully branded and quick to launch
- Easy to integrate - no rip-and-replace
- Proven to drive measurable engagement and ROI
- Scalable across both mid-market and large ASO clients
We’re your dedicated partner, from sales enablement to account management, implementation, and reporting, we’re in your corner every step of the way.
Have a group in mind or want to see what’s new?
We’d be happy to connect and walk through the latest enhancements.
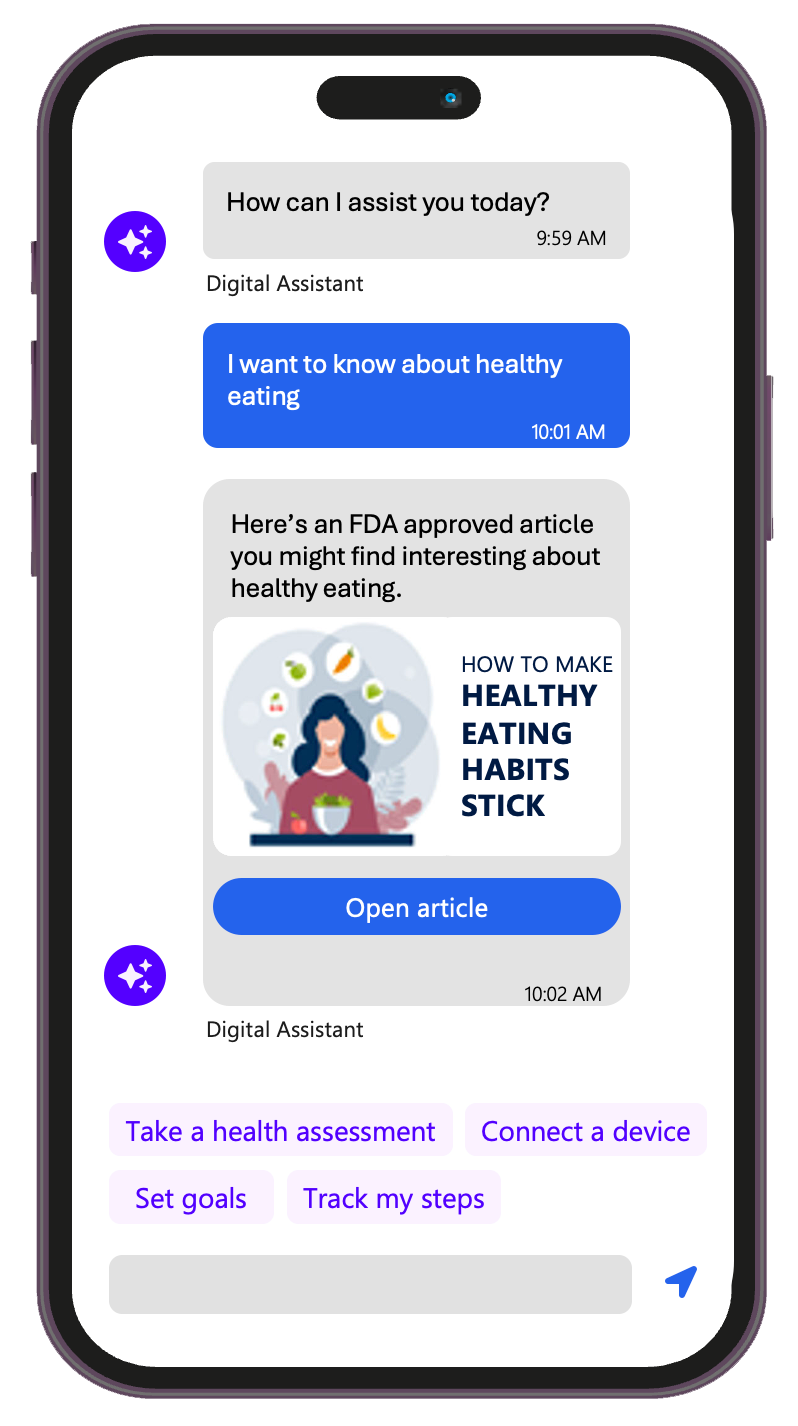
AI Wellness Agent – Smart, Personalized Health Navigation
Available NowYour members have questions. Our AI Wellness Agent has answers – fast.
With enhanced natural language understanding and user intent recognition, this digital guide simplifies access to wellness resources, surfaces relevant next steps, and intelligently routes emergencies. Tailored support meets members where they are in their wellness journey.
ReallyWell℠ Challenges Enhancements – A More Engaging Experience
UI and Data Improvements Available in August with full new experience available in JanuaryWe’re enhancing the ReallyWell℠ Challenges experience to drive greater member engagement and satisfaction. Updates include real-time display of synced device data, personalized challenge recommendations based on health assessment results, clearer progress tracking, and visual indicators for new challenges introduced during the plan year.
Combined with refreshed UI elements that resolve confusion and improve usability, these enhancements make it easier and more motivating for members to stay on track with their wellness goals.
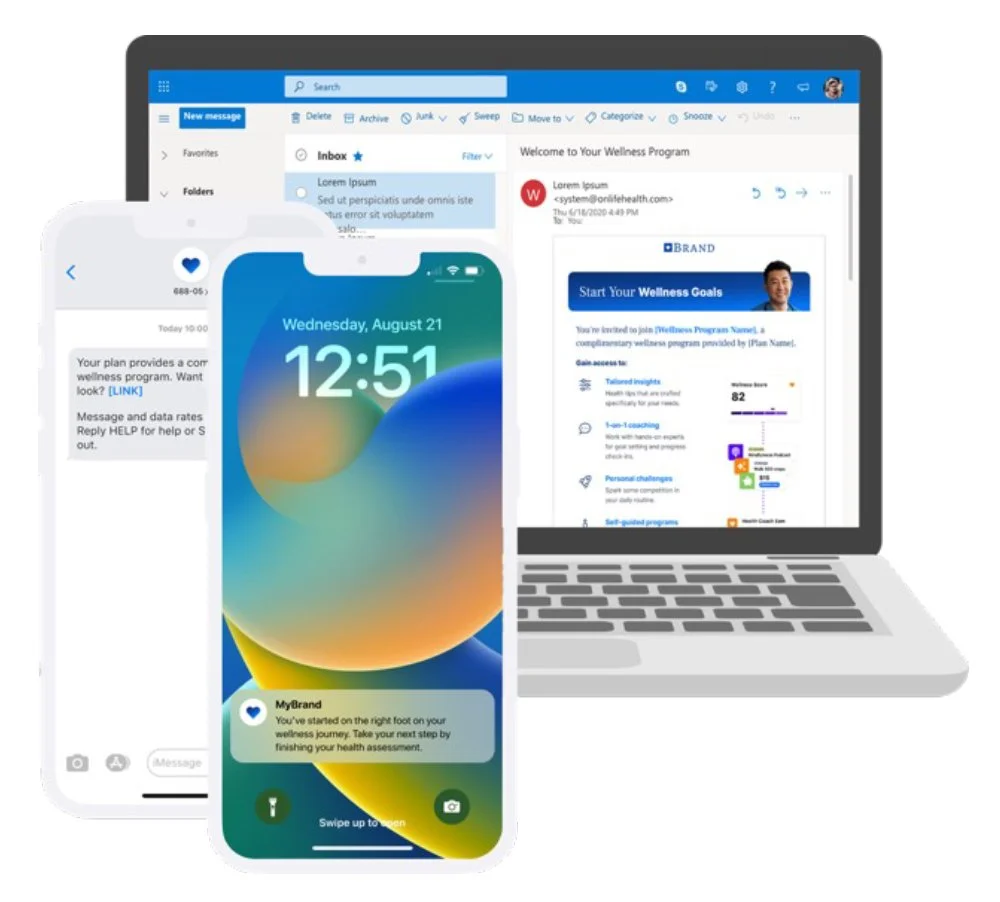
Engagement Messaging: Deep Linking – Drive Seamless Member Journeys
Available in August We’re making it easier than ever for members to get where they need to go with the launch of Deep Linking. This enhancement ensures that external links from emails, texts, and campaigns route users directly to the right in-app content – like a specific article, challenge, or self-guided program – instead of a generic landing page.
With support across web, iOS, and Android, deep linking delivers a more consistent, frictionless experience that boosts engagement, reduces drop-offs, and increases the effectiveness of your marketing campaigns. It also enables better tracking, attribution, and campaign control – helping teams drive repeat usage and measurable value.
Call to Chat – Bridge the Gap Between Voice and Digital Support
Available in SeptemberLong wait times and limited support hours frustrate members who call in for help. Our new Call to Chat feature allows members to seamlessly shift from a phone call to chat-based support, maintaining continuity in the conversation and reducing drop-off.
Whether it's after hours or during peak times, this tool ensures members stay engaged and connected to care – when and how they need it.
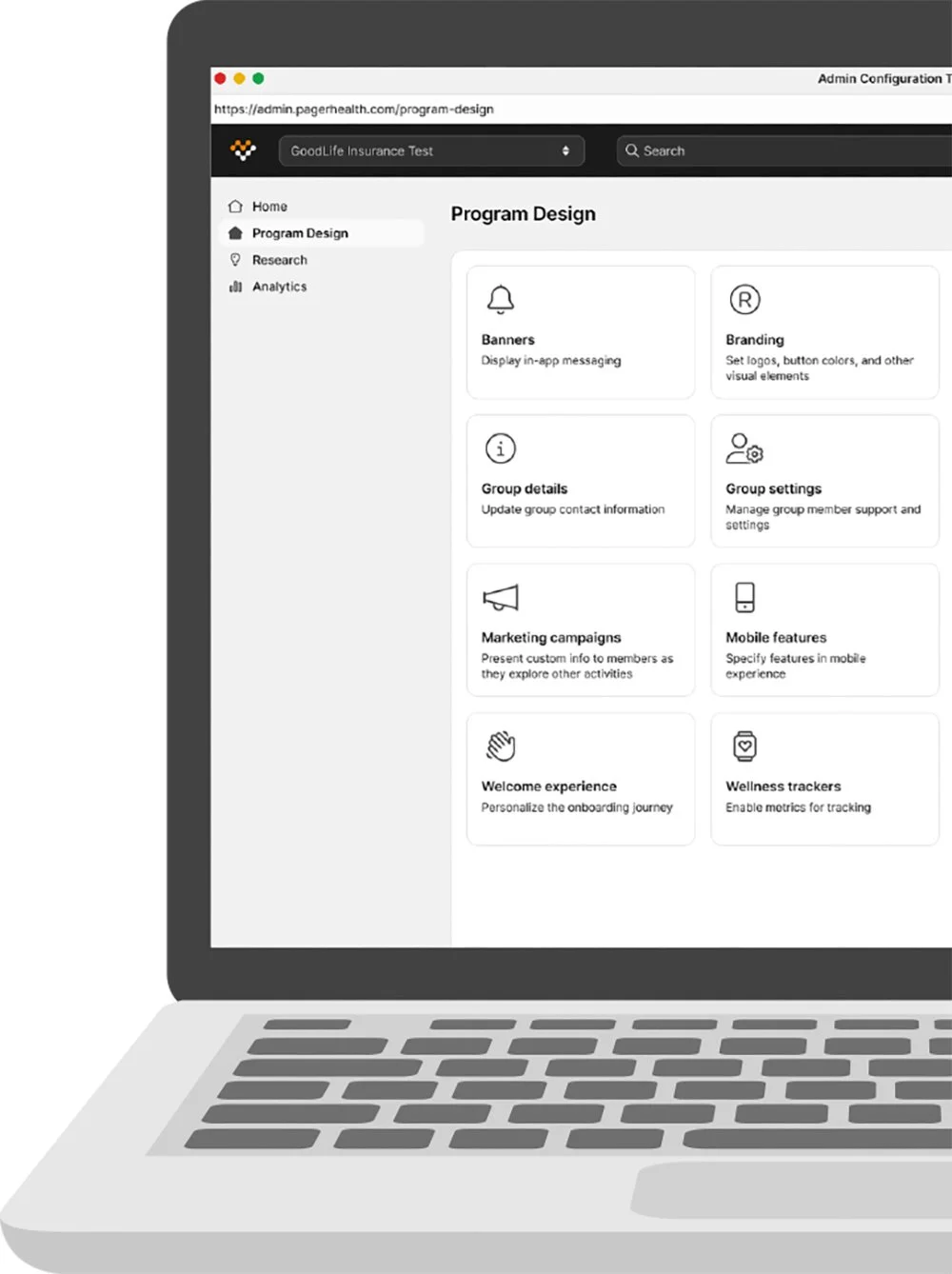
Admin Config Tool – Self-Service Control for Wellness Group Management
Available in early Q4Health plans need flexibility and speed when managing their wellness programs. Our new Admin Config Tool empowers clients with real-time, self-service access to key configurations – starting with wellness group setup. By eliminating the need to submit support tickets for common adjustments, this tool gives plans direct control to design and manage differentiated experiences for their members, faster and more efficiently.
ACT isn’t just a tool - it’s how we help health plans deliver efficiency, customization, and control at scale.
Looking Ahead
With deep linking, configurable tools, and AI-powered agents now live or launching soon, we’re laying the foundation for a smarter, more connected member experience. As we head into Q4, we’ll continue expanding self-service capabilities, enhancing personalization, and equipping clients with the tools they need to deliver differentiated, value-driven solutions. Stay tuned – even more innovation is on the way.
If you want to learn more about Pager Health’s new and exciting features, please reach out to your Pager Health sales or account management executive.