25%
lower care cost
50%+
call deflection
3.3x
projected ROI
Next-generation care navigation,
powered by AI and backed by clinicians
Deliver a unified, AI-powered care experience that’s safe, scalable, and entirely app-free.
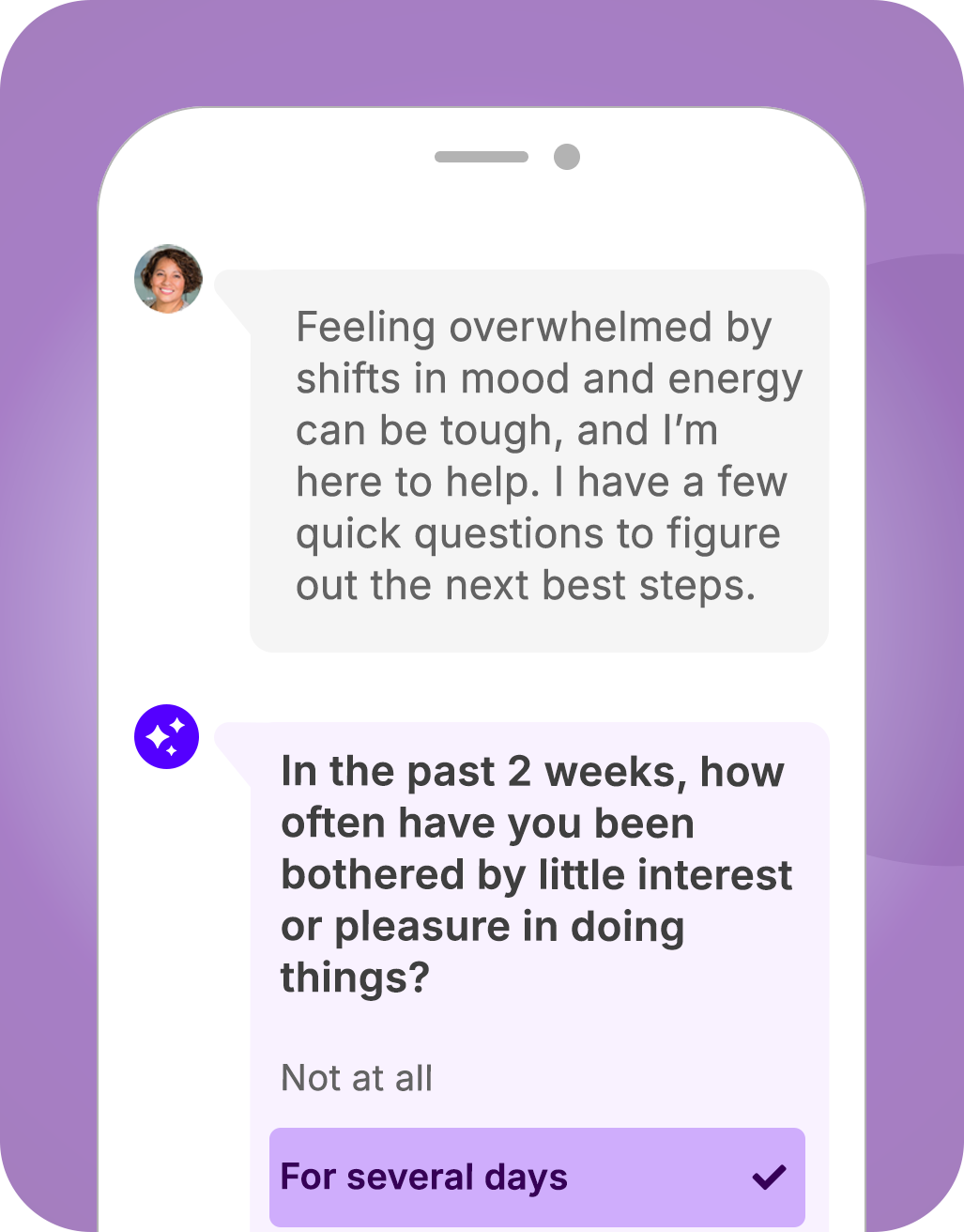
Clinical Navigator
On-demand clinical triage
Modernize nurse lines into a 24/7 telephonic and digital, AI-enhanced experience that guides members to the right care fast (URAC-accredited clinical operations)
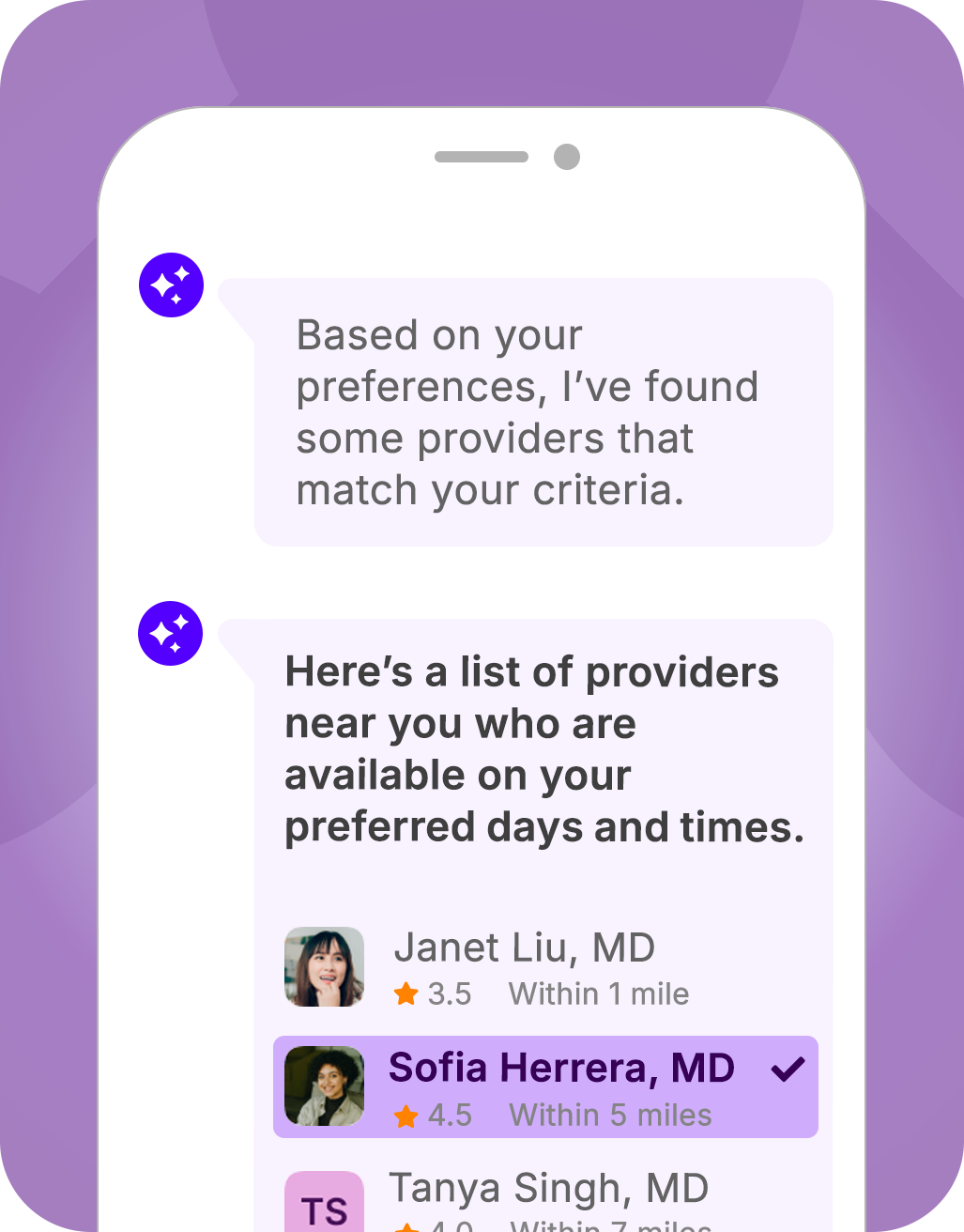
Provider Navigator
Provider finder and scheduling
Improve network performance and reduce care delays with conversational provider search and one-click scheduling – without EHR integrations
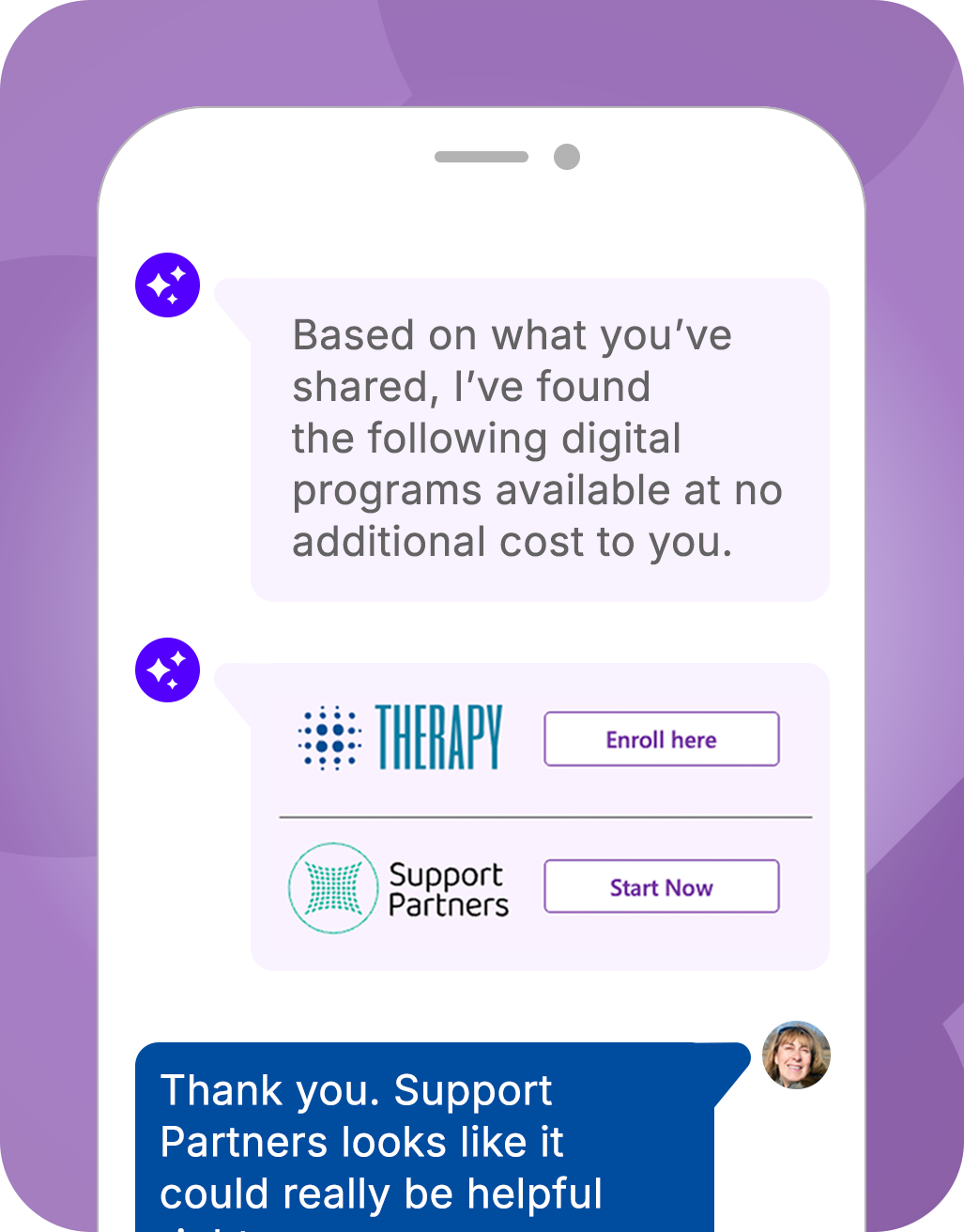
Program Navigator
Digital health program guidance
Increase program utilization with intelligent triage and AI-powered program matching to guide members to in-network program and support
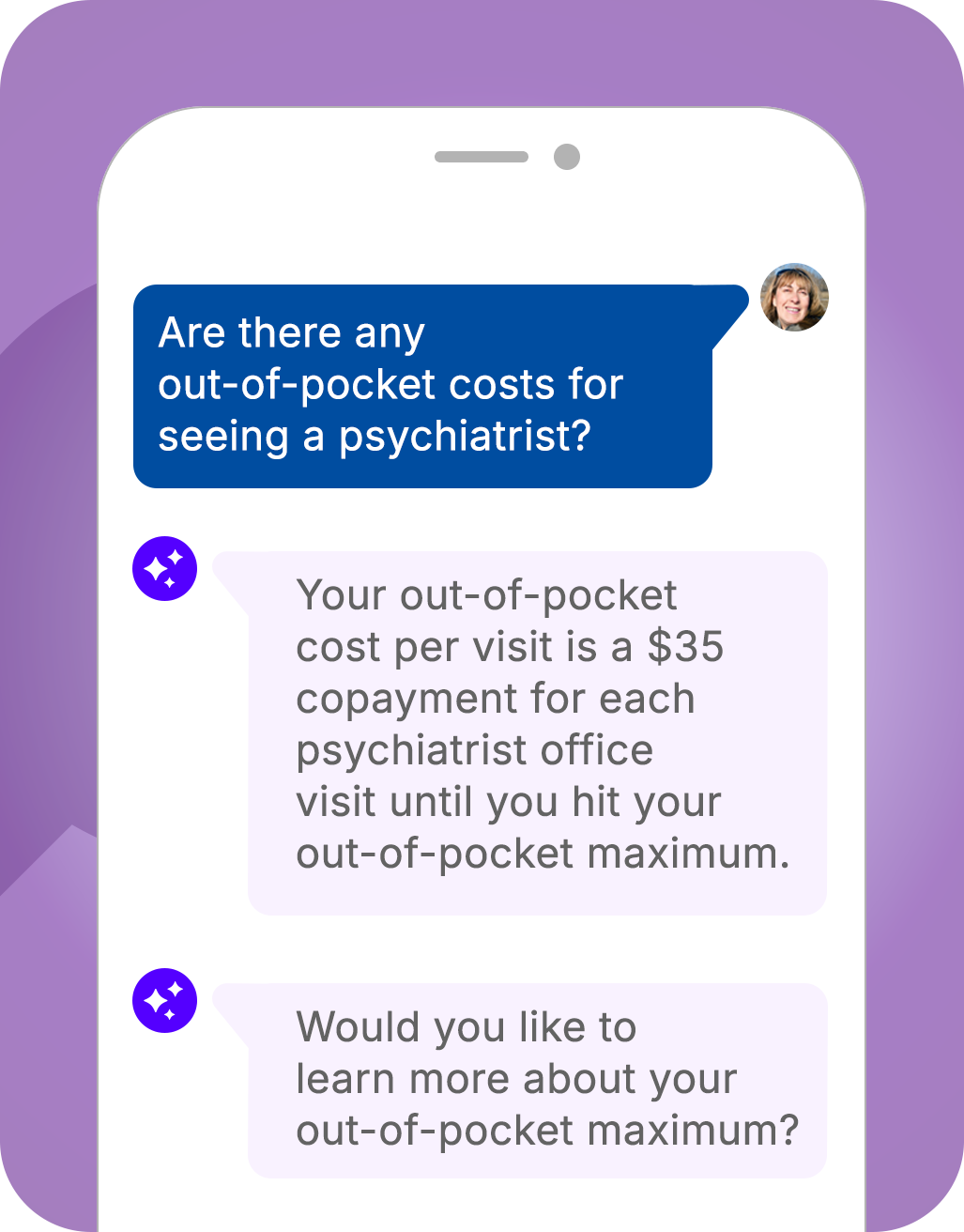
Intelligent benefit assistance
Benefit Navigator
Go beyond conversational FAQ chatbots with a navigation-driven AI agent that resolves member questions and drives action
See Pager Health℠ Navigator in action.
Discover how our innovative solutions translate to meaningful operational efficiency, improved care navigation, and measurable ROI.
Healthcare is fragmented. Navigator unites it.
Health plans face rising costs and underused benefits. Pager Health Navigator enables health plans to unify the care journey, simplify access, and improve outcomes. All without disrupting existing plan infrastructure.
Unified navigation:
One experience for benefits, providers, point solutions, and clinical support
Omnichannel access:
Members can initiate care needs via secure chat, SMS, voice, video, or member portal
Proactive engagement:
Outreach to activate preventive and condition-specific programs
AI first, human always:
Smart automation backed by licensed RNs (URAC accredited)
Seamless integration:
Connects with existing plan systems and partner solutions
Smarter tools for better health
AI-powered symptom triage and routing
In-network provider finder with scheduling assistance
Benefit and coverage guidance personalized to the member
Digital health program matching (behavioral, chronic, episodic)
Aftercare and follow-up to drive outcomes
24/7 Nurse Navigation and escalation
93%
use of high-performing providers
99%
health issues resolved after initial interaction with nurse
3.3x
increase in care gap closure
Great healthcare starts with a conversation
Discover how our innovative solutions can bring your digital health vision to life.